Introduction
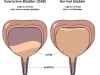
The overactive bladder is characterised by a set of symptoms such as an uncontrollable urge to pass urine and the frequent need to urinate both during the day and at night. It may also be associated with urge incontinence (urine leakage when one cannot get to the toilet in time due to an overwhelming urge).
OAB impact on quality of life
OAB can significantly impact on someone’s quality of life emotionally, socially, physically, and financially. Patients find their lives revolving around the toilet and they must plan their day according to access to a toilet. Some people avoid social situations due to fear of leaking, smell, and embarrassment. This can happen to the extent that some rarely leave the house and become a ‘bladder hermit’.
Sufferers often feel tired all the time because they wake up too many times at night to pass urine and are therefore not getting enough rest.
They are unable to enjoy a normal diet as they must restrict both solid and fluid intake in order not to trigger a bladder spasm.
Financially, the costs of pads or bladder medications can add up to a significant amount. All these culminate in a sense of loss of control over the bladder and eventually, one’s life.
Symptoms of OAB
Ask yourself these questions. You may suffer from an overactive bladder if these symptoms are familiar to you.
- Do you have a sudden need to rush to the toilet to urinate?
- Is this precipitated by hand washing or turning the key in the front door?
- Have you not made it to the toilet fast enough and leaked urine?
- Do you pass urine many more times than others during the day?
- Do you always have to know where the toilet is when you are out of the house?
- During the night, does your bladder wake you up multiple times?
If you have been diagnosed with OAB, take the validated International Continence Society (ICS) questionnaire on OAB – ICIQ-OAB, to assess its severity and impact on quality of life.
What causes OAB?
Most commonly, there is no known cause for OAB (idiopathic). Some cases are related to a neurological cause such as Parkinson’s, multiple sclerosis, or strokes. OAB can also occur secondary to an obstruction of the bladder outlet such as prostatic obstruction in men (see benign prostatic hyperplasia).
How common is OAB and is it treatable?
OAB is very common. 1 in 6 people suffer from it, and it can occur even in young healthy people. However, the incidence increases with age. It is often thought to be more common in women but in reality, it is just as common in men. Many people do not seek medical attention and decide to just ‘live with it’. This is unfortunate because there are now a lot of effective treatment options available. Many of these options are now subsidised by Medicare (including anti-spasm bladder injection and sacral neuromodulation).
What other conditions can be mistaken for an OAB?
- Urinary tract infection
- Interstitial cystitis
- Bladder cancer
- Bladder stone
- Polyuria (excessive production of urine by the kidneys)
What are the investigations?
- A urine test is done to rule out a urinary tract infection.
- A bladder diary is a useful method of quantifying urinary frequency, volume voided, fluid intake, and leakages. A patient with OAB will show frequent, small voids.
- A questionnaire (ICIQ-OAB) can be done to get an unbiased assessment of the impact of OAB on a patient’s quality of life. It can also be used to measure treatment outcomes.
- X-ray imaging is not done routinely, but a kidney ultrasound or CT scan can be useful if:
- History of possible neurogenic bladder.
- History of pain or blood in the urine.
- Suspicion of anatomical abnormalities.
- A urinary tract ultrasound can measure prostate size (in men), and the volume of urine left in the bladder after a void.
- A cystoscopy is not done routinely unless:
- Suspect bladder cancer (history of blood in the urine).
- Bladder pain (rule out bladder pathology like stones or interstitial cystitis).
- Significant obstructive symptoms (poor flow, straining).
- Urodynamics or bladder function study is indicated in patients:
- With complex history.
- Neurogenic bladder.
- Mixed incontinence (both stress and urge incontinence).
- Previous pelvic or incontinence surgery.
- Not responding to medications or diagnosis unclear.
- Before invasive surgery.
- With complex history.
What are the treatment options?
Treatments should always start from conservative ones to more invasive ones.
Conservative treatments
- Lifestyle changes (reduce caffeine and alcohol).
- Behavioural therapy (bladder retraining).
- Medications.
Medications
Anticholinergic drugs
Medications are the mainstay of conservative treatment options. Anticholinergic drugs are most commonly used. They act by ‘calming’ down bladder activity. Common side effects include dry eyes (blurred vision), dry mouth and constipation. Other side effects are confusion, dizziness, rapid heartbeat, and urinary retention (unable to pass urine). Patients with glaucoma should check with their ophthalmologist (eye doctor) before starting on these drugs. These medications achieve maximal effect after 2 to 3 months and hence should be encouraged for that duration before concluding they are not effective.
There are now many drugs in this category such that to a lay person, it may seem confusing. They differ in the number of times taken per day, mode of administration, side effect profile, efficacy, and cost. Some of the medications have fewer side effects but are not subsidised by Medicare and hence, are more expensive. Your doctor should be able to discuss with you, which drug is the most appropriate one.
Beta 3 Agonist
Beta 3 agonist (Mirabegron) medication acts via a different pathway compared to the anticholinergic drugs, to treat the overactive bladder. It tends to cause fewer side effects and is very well tolerated. Uncommonly, it may cause a slight rise in the blood pressure or palpitation.
Alpha-blockers
In men with OAB secondary to obstruction from an enlarged prostate, another class of drugs may be tried first (alpha-blockers) to relieve the obstruction. Sometimes, this will indirectly result in an improvement of the OAB symptoms over time. In those that don’t, an anticholinergic or beta 3 agonist medication can be added to treat the OAB symptoms.
Surgery
Minimally invasive surgical treatments
In the past, surgical options are highly invasive and involve major surgery. The advent of minimally invasive techniques (anti-spasm bladder injection and sacral neuromodulation) has revolutionised the treatment of drug-refractory OAB (those not responsive to medications).
- Anti-spasm bladder injection
- This has now been approved by PBS in Australia for patients with the neurogenic bladder (spinal cord injury, spina bifida, multiple sclerosis) and idiopathic OAB (from Nov 2014).
- This outpatient procedure is done during a cystoscopy and takes about 15 minutes to do. It is effective in about 70% - 95% of patients.
- The effects wear off over time, and patients would need a ‘top-up’ every 6 to 9 months.
- Sacral neuromodulation (bladder pacemaker)
- Involves 2 stages; a trial stage and an implant stage.
- A small electrode is first inserted into the lower back (sacral spine) to lie next to a sacral nerve root.
- This trial stage lasts about 2 weeks and if the patient shows improvements in symptoms, then a permanent battery is implanted.
- PTNS (posterior tibial nerve stimulation)
- Non-invasive treatment involves placing a stimulating electrode on the skin on the foot, overlying a nerve that can indirectly affect bladder control.
- Need multiple treatments (usually once a week initially, then once a month for maintenance).
- Performed in the medical practice office.
Major surgical treatments
- Augmentation cystoplasty
- A piece of small bowel tissue is reflected and sutured onto an opened bladder to create an ‘augmented’ bladder in terms of volume that can maintain a lower pressure within it.
- Overactive bladder contractions are dissipated over this larger volume and become less symptomatic and less dangerous to the kidneys.
- Patients may need to learn to do intermittent self-catheterisation if the bladder does not empty well.
- The bowel segment of the augmented bladder will continue to produce normal mucous, which will mix in with normal urine.
- There is an increased risk of bladder stone formation.
- Routine yearly cystoscopy would have to be performed, as there is a very small risk of the bowel segment undergoing malignant transformation over time.
- Urinary diversion
- This is usually done as a last option.
- Urine can be surgically diverted by implanting the ureters (tubes draining the kidneys to the bladder) into a piece of small bowel. This then exits to the abdominal skin surface (stoma) into a bag.
Long-term indwelling catheterisation
Some frail patients may not be suitable for any of the above treatment options. A long-term indwelling catheter may be the best option in this case.
Related information
Read A/Prof Gani’s publication - Rebooking methods can cause delays in a patient’s treatment:
Download Busting for botox an analysis of rebooking methods and delay to reinjection of intravesical botulinum toxin a - PDF (174 Kb)
Read A/Prof Gani’s publication:
Download Modifications to botulinum toxin a delivery in the management of detrusor overactivity recalcitrant to initial injections - PDF (904 Kb)
Read A/Prof Gani’s publication:
Download Position statement a clinical approach to the management of adult non neurogenic overactive bladder - PDF (260 Kb)
Read A/Prof Gani’s publication - SNM is a reasonable treatment option for patients
Download Sacral neuromodulation for detrusor hyperactivity with impaired contractility - PDF (1500 Kb)
Read A/Prof Gani’s publication:
Download Sacral neuromodulation for refractory overactive bladder after prior intravesical onabotulinumtoxina treatment - PDF (124 Kb)